Description
Renal dialysis solutions play a crucial role in the management of patients with kidney failure, serving as artificial means to filter and purify blood when the kidneys can no longer perform these functions effectively. There are two primary types of dialysis: hemodialysis and peritoneal dialysis, each utilizing specific solutions that cater to different physiological mechanisms. In hemodialysis, a dialysis fluid, known as dialysate, is carefully formulated to draw waste products, excess electrolytes, and toxins out of the blood while adding essential components. The composition of dialysate typically includes electrolytes such as sodium, potassium, and bicarbonate, which can be adjusted to meet the individual needs of the patient, ensuring proper electrolyte balance and acid-base homeostasis during the procedure.
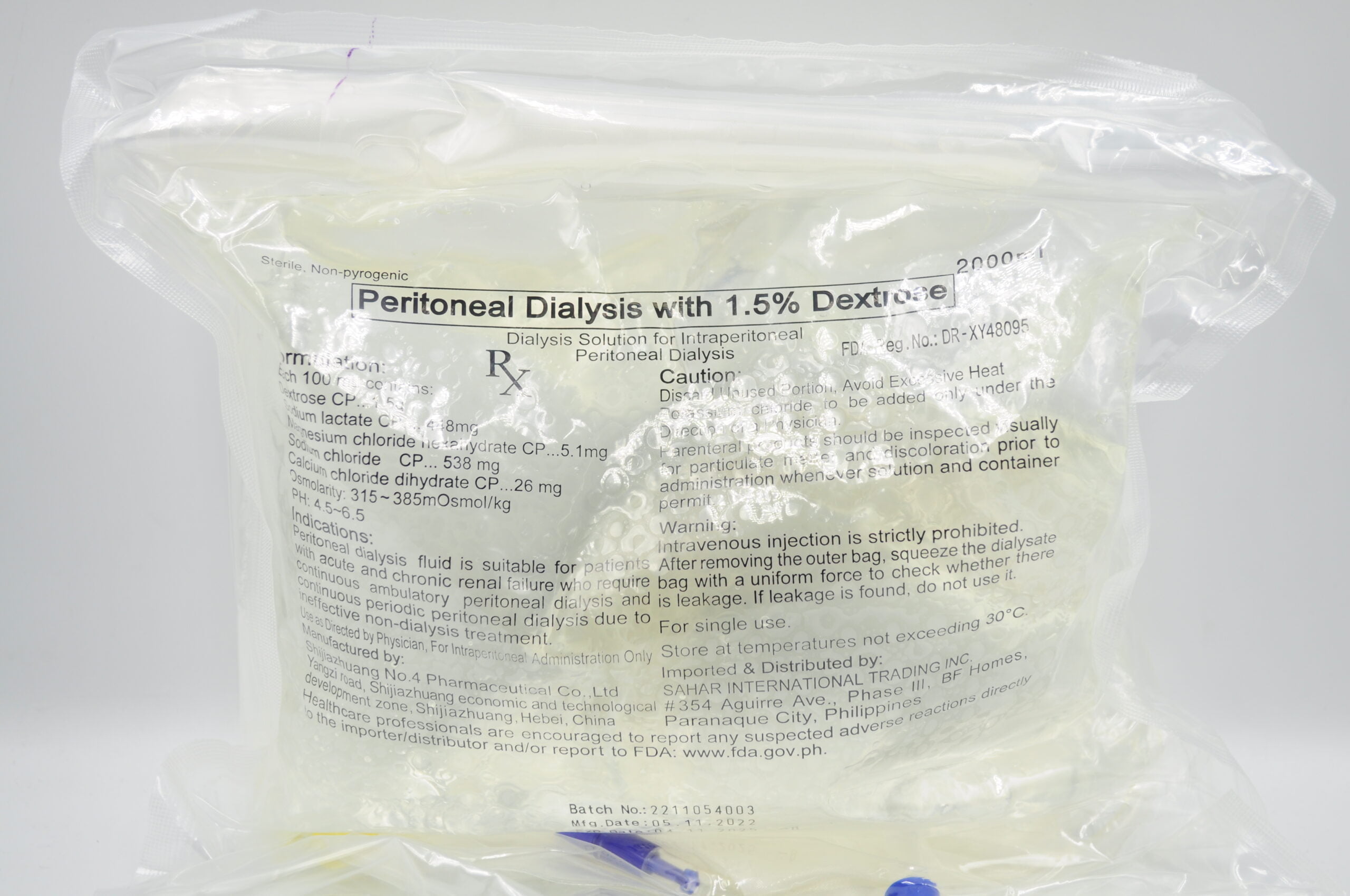
On the other hand, peritoneal dialysis employs a different approach, using a sterile solution that is introduced into the abdominal cavity, where it interfaces with the peritoneal membrane. This dialysis solution is isotonic and contains glucose or dextrose, which creates an osmotic gradient that facilitates the removal of waste products and excess fluid from the bloodstream into the cavity. The dialysate in peritoneal dialysis is usually exchanged multiple times a day, allowing for a more continuous clearance of toxins, making it a patient-friendly option that can be performed at home. Both types of dialysis solutions are essential in optimizing the treatment process, enhancing the quality of life for patients with chronic kidney disease, and managing the complications that arise due to renal impairment.
The formulation of renal dialysis solutions is an ongoing area of research, with advances aimed at improving biocompatibility and minimizing side effects. Innovations in dialysis solutions intend to reduce the risk of complications such as infection, inflammation, and electrolyte imbalances. Additionally, customized solutions that take into account individual patient characteristics, such as comorbidities and lifestyle factors, are becoming increasingly more common, enabling healthcare providers to tailor dialysis regimens that maximize therapeutic effectiveness while enhancing patient compliance and satisfaction. As our understanding of renal physiology and the intricate dynamics of dialysis improves, the field continues to evolve, presenting opportunities for better management of renal failure and ultimately improving patient outcomes.